Implanting beta cells has been a promising, yet problematic approach to treating diabetes. These cells live in the pancreas and, in healthy people, secrete vital insulin to regulate blood sugar levels. But in sufferers of diabetes they don't quite work as required. Building on previous work on a smart insulin patch, scientists have now discovered a way of delivering the effects of these cells in a way that overcomes some of the complications.
For decades, scientists have been exploring beta cell transplants as a way of getting diabetes sufferers the insulin they need, without the 24-hour monitoring and uncomfortable injections. While hundreds of these procedures have been carried out, only a fraction of them are successful. This is because the recipient's immune system often rejects the foreign cells, and while drugs can be taken to suppress these attacks, they can also spoil the effectiveness of the freshly implanted cells while they're at it.
So researchers at the University of North Carolina (UNC) at Chapel Hill and North Carolina State University set out to develop a device that would keep these beta cells beyond the grasps of the immune system, but still capable of performing their role. Their latest work actually builds on a device they unveiled last year, described as smart insulin patch. This patch was designed to mimic the effects of the body's beta cells, by releasing tiny insulin bubbles into the bloodstream when required through more than 100 microneedles.
Instead of loading the microneedles, each about the size of an eyelash, with insulin, this time around the researchers filled them with thousands of live beta cells. These cells were protected in tiny capsules made from a biocompatible alginate. When the patch – made from materials commonly used in cosmetics and diagnostics and about the size of a quarter – is stuck onto the skin the needles puncture the capillaries and blood vessels, creating a direct channel between them and the cells of the patch.
But forging this connection was only half the battle in developing the responsive smart patch. The researchers also created what they called glucose-signal amplifiers. These are synthetic nanovesicles filled with chemicals that enable them to recognize rising blood sugar levels and release insulin where needed.
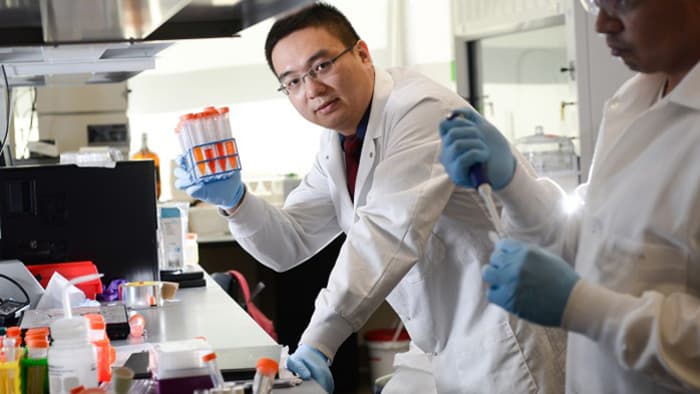
"This study provides a potential solution for the tough problem of rejection, which has long plagued studies on pancreatic cell transplants for diabetes," said senior author Zhen Gu, PhD, assistant professor in the joint UNC/NC State department of biomedical engineering. "Plus it demonstrates that we can build a bridge between the physiological signals within the body and these therapeutic cells outside the body to keep glucose levels under control."
The team put their new smart patch to work on animal models of type 1 diabetes. They found that mice wearing the patch had skyrocketing blood sugar levels significantly lowered for 10 hours at a time. They also applied a second patch to investigate whether it would force blood sugar levels to dangerously low levels, a condition known as hypoglycemia. Promisingly, they found that it didn't cause excessive dosages of insulin, rather it lengthened the life of the treatment to 20 hours.
Rather than a set and forget-type treatment, the researchers say with further development smart insulin patches could complement existing approaches to make life much easier for diabetes sufferers. They say their results provide a proof-of-concept for an easier approach, but more tweaking, pre-clinical test and then human trials are needed before we see them in use.
"Managing diabetes is tough for patients because they have to think about it 24 hours a day, seven days a week, for the rest of their lives," says co-author John Buse, professor of medicine at the UNC School of Medicine. "These smart insulin approaches are exciting because they hold the promise of giving patients some time off with regards to their diabetes self-care. It would not be a cure but a desperately needed vacation."

 Previous page
Previous page Back to top
Back to top







